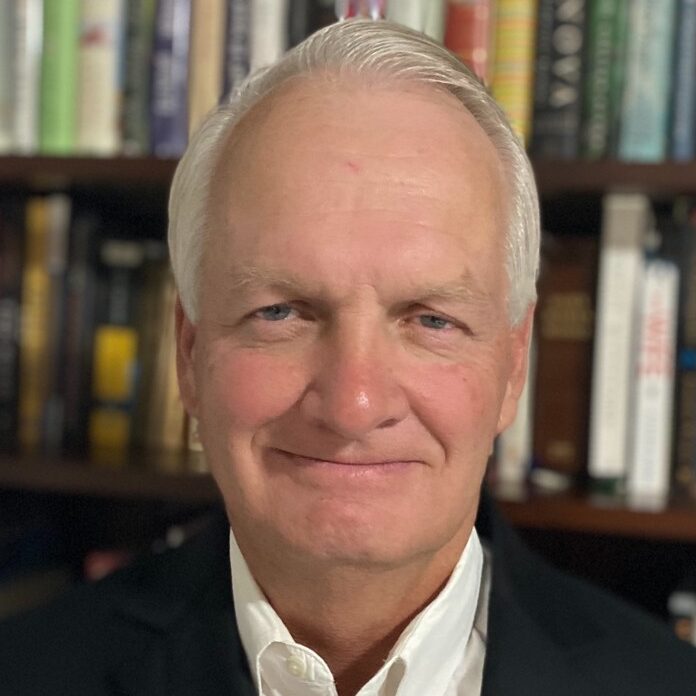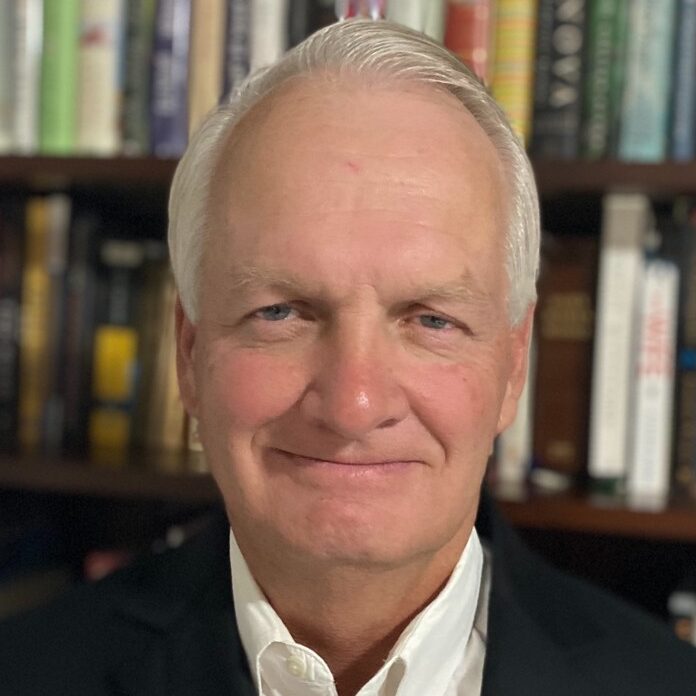
Chris is a Healthcare Executive with 40 years of experience in C-Suite and Director level roles. He has been a member of several senior management teams with direct responsibility for revenue cycle, supply chain, treasury operations, reimbursement, financial reporting, financial planning, internal auditing, information systems, construction project oversight, oversight of all joint ventures, and oversight of all malpractice claim settlements and lawsuits.
Sub-Specialties
- Experience with academic adult, academic children, large non-academic referral, and community hospitals
- Provider/payer relations
- Employment and integration of academic and private physician practices
- Performance and margin improvement
- Revenue and supply chain restructuring
- System integration, acquisition, and divestiture strategies
- Former CFO Methodist Le Bonheur Healthcare
Professional Experience
- Senior CFO Consultant – Warbird Consulting Partners
- Director Consulting Services – E78 Partners
- Director of Finance and Administration – Shelby County Government
- Methodist Healthcare
- Executive Vice President and Chief Financial Officer
- Chief Financial Officer – Memphis Division
- Chief Financial Officer – Mississippi Division
- Chief Financial Officer – Wellmont Health System
- Chief Financial Officer – Holston Valley Health Care, Inc
- Promoted various times (Financial Analysis to Director) – Methodist Health Systems
- Senior Accountant Regulatory Affairs – Houston Lighting & Power Co.
- Budgeting and Audit Analyst – Caterpillar Tractor Company
Professional Accomplishments
Bond ratings improved from BBB+ to AA- by S&P and from Baa1 to A1 by Moody’s due to improved margins and balance sheet ratios. Operating margins were consistently positive since 2000 and key balance ratios have steadily improved with days cash increasing from 73 to 234 and cash to debt ratio from 0.4 to 1.75. Total revenues for the system have steadily grown from $0.8 billion in 2000 to $2 billion in 2018
Restructured revenue cycle process which included the formation of a central business office for all hospitals and physician practices, reduced denials, reduced managed care underpayments, and lowered net days in accounts receivable to mid 40’s
Restructured supply chain process which resulted in reduced number of vendors, reduced prices from remaining vendors, increased use of technology such as bar codes and electronic invoicing & payments, and improved satisfaction levels of clinical areas
Led transition from Premier purchasing group to Parallon/Health Trust group reduced supply costs by $15 million annually
Oversaw the implementation and growth of 340b drug program which resulted in annual savings growing from $1 million in 2004 to over $115 million in 2018
Redesigned malpractice settlement process to focus on early communication with patients and families, centralization of all claims with one legal firm, focused follow up of all open claims to ensure timely resolution, and improved reporting of identified risk issues across the System to ensure process improvements are implemented across all facilities. Changes resulted in malpractice liability being decreased from $75 million to $20 million
Led a cost reduction processes at numerous health systems that led to reductions of over $100 million
Negotiated limited network managed care contracts with Cigna, United and Blue Cross which increased managed care market share to over 50%
Actively involved in physician integration strategies with private and academic physicians that have resulted in either employment or professional service arrangements with over 490 physicians